Spotlight On: Hysteroscopy

 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Hysteroscopy Special Interest Group (SIG) led by Chair, Alka Kumar, MBBS, MS.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Hysteroscopy Special Interest Group (SIG) led by Chair, Alka Kumar, MBBS, MS.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
NEW to SurgeryU!!! SIG Recommended SurgeryU Video #1:
Hysteroscopic Myomectomy of Large Submucous Fibroid
By Tanvir Tanvir, MBBS, MS and Alka Kumar, MBBS, MS
Hysteroscopic myomectomy using the slicing technique with resectoscope is the standard of care. Large fibroids of size > 4 cm, usually require two procedures. This video demonstrates hysteroscopic myomectomy of a 4.5 cm FIGO type 0 submucous fundal fibroid, using hysteroscopic tissue removal system in a single step. The viewer will be able to learn about the technique of myomectomy with HTRS and the importance of right case selection, as demonstrated in this video.
SIG Recommended SurgeryU Video #2:
Hysteroscopy for Retained Products of Conception
By Caitlin A. Jago, MD, Brittany Kathleen MacGregor, MD, Dong Nguyen, MD, FRCSC, Sukhbir Sony Singh, MD, FRCSC
Retained Products of Conception (RPOC) are a relatively common occurrence after any pregnancy outcome. Clinical management, including the diagnosis, as well as treatment, remains a challenge. Hysteroscopy plays an important role in the improvement of both diagnosis and management, as well as outcomes, especially in populations with fertility challenges, but it is still not used as widely as it should be for this indication. This video effectively summarizes different techniques for removal of RPOC.
SIG Recommended SurgeryU Video #3:
Not Always A Slam Dunk, Evaluation of Asherman’s in a Patient with Retained POC
By Michelle Gruttadauria, MD and Megan Loring, MD
There is significant overlap between intrauterine adhesions and retained products of conception. It is debatable what is the cause and what is the consequence, but an association is certainly present. This video is a great reminder to perform a second look follow up after treatment of RPOC, especially in patients with history of intrauterine adhesions.
JMIG Article Recommendation #1:
Cervical Septum Incision Adversely Impacts Clinical Outcomes in Women with Complete Uterine Septum and Duplicated Cervix
Ninghong Jiang, MD, PhD, Yu Xie, MD, PhD, Wenjie Qu, MD, Lei Lei, MD, Shujun Gao, MD, PhD, Hongwei Zhang, MD, Qing Wang, MD, Limei Chen, MD, PhD and Long Sui, MD, PhD
This article provides an evidence-based approach on very real clinical decision making regarding whether or not to incise the cervical septum when resecting a complete uterine septum. A few years ago, I myself asked four hysteroscopy experts for advice on this very question, and they were divided 50/50 in their approach to resect, or not to resect, the cervical portion of the septum.
JMIG Article Recommendation #2:
Prostaglandin Injection for Myoma Expulsion (PRIME): Case Series of a Novel Approach to Hysteroscopic Resection of FIGO Type 2 Myomas
Sarah C. Cromack, MD, Lulu Yu, MDb, and Magdy P. Milad, MD, MSb
Complete resection of fibroids in one procedure, by hysteroscopic myomectomy, remains a challenge, especially when dealing with larger and deeper imbedded (FIGO type 2) submucosal fibroids. This article, even though done on small number of patients, provides a novel idea to consider to improve chances of complete resection.
A Message from the SIG Chair:
Hysteroscopic Markers of Endometrial Tuberculosis
A tuberculosis outbreak in Kansas City was reported in January 2025 with 67 confirm cases of active tuberculosis disease and 79 confirmed latent tuberculosis cases. [1- 4]
In 2016, in Southeast Asia, there were almost three million cases of tuberculosis (TB), and 15% manifest as extrapulmonary. [5] TB can emerge multi‑organ, including the female genital tract. The latter one is the iceberg phenomenon that would affect women’s life quality. The incidence of female genital tuberculosis (FGTB) varies from 1% to 21%. [6] Hysteroscopy is considered a tool to obtain FGTB signs and biopsy. Many past studies have considered fluid hysteroscopy to be a reliable and useful examination for investigating endometrial tuberculosis [7-16].
Clinical presentations of endometrial tuberculosis are often subtle or mimic other gynaecological disorders. Infertility and chronic lower abdominal pain are common symptoms. Tubal and endometrial involvement in genital tuberculosis frequently precludes spontaneous conception, making assisted reproductive technologies also challenging. Diagnosis is based on being a paucibacillary disease, demonstration of mycobacterium tuberculosis is not possible in all cases. Various blood tests, nonspecific tests, serological (e.g., PCR), sonoradiological investigations like USG, HSG, and MRI have been tried to diagnose this disease.
Key reproductive implications include:
- Tubal Dysfunction: Tubercular inflammation (endosalpingitis, perisalpingitis) causes blockage, adhesions, and loss of tubal functionality, potentially forming tubo-ovarian masses.
- Endometrial Changes: Endometrial damage may manifest as synechiae, granular ulcers, ostial fibrosis, and obliteration of the uterine cavity.
- Endometrial Changes
- Immune Dysfunction
The impact on reproduction is profound, complicating spontaneous conception and assisted reproductive technologies (ART). Embryo implantation failure occurs frequently due to disturbed endometrial receptivity. Mechanisms involved include impaired immunological markers essential for implantation, disrupted vascularization due to immunomodulation (vascular thrombus formation, antiphospholipid antibody activation), reduced sub-endometrial blood flow, and direct endometrial atrophy leading to adhesion formation (synechiae).
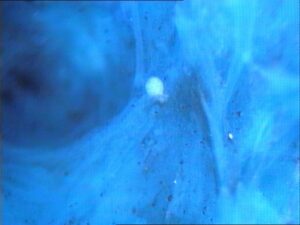
Hysteroscopic Markers of Endometrial Tuberculosis – As Seen on Diagnostic Hysteroscopy Are:
- A rough, pale, uneven endometrial surface lacking clear glandular openings, often described as dirty or bizarre in appearance. [7-16]
- Whitish, tubercular deposits varying from microscopic granules to large macroscopic lesions. [7-16]
- Ill-defined gland openings and intrauterine adhesions (synechiae). [7-16]
- Starry Sky Appearance [10]
- Adhesions
Classical hysteroscopic findings of endometrial tuberculosis is a rough, dirty looking, bizarre, pale endometrium with gland openings not seen and with overlying whitish deposits [7-11, 14,15] and adhesions. Endometrial scarring on Hysteroscopy is one of the pathognomic features in endometrial tuberculosis especially if whitish deposits overlying the endometrium are also seen. Endo cervical scarring is also frequently seen in endometrial tuberculosis.
In endometrial tuberculosis intraluminal adhesions in the interstitial part of the fallopian tube can often viewed at hysteroscopy by placing the microhysteroscope tip very close to the tubal orifice and viewing with a source magnification of 25x.
At times panoramic hysteroscopy with 1x magnification using a conventional telescope (27005 BA; Karl Storz GmbH & Co., Tuttlingen, Germany) reveals an endometrium unremarkable except for subtle scarring, which could also be overlooked. The endometrium is next visualized using a Hamou Micro-Hysteroscope II (26157 BT; Karl Storz) [6,9] in the panoramic view at 20x at-source magnification, which reveals a rough-looking endometrium as though it had been sprinkled with a coarse whitish powder. The endometrial surface is bumpy, with diffusely scattered small conical papillary projections, and no endometrial glands are observed.
Hysteroscopic visualization of the endometrium after antitubercular therapy often shows an improvement in the mucosal morphology. Relook hysteroscopy after anti tubercular therapy guides the surgeon towards prognosis and results of anti tubercular therapy.[11]
 |
 |
| A Tubercular deposit resting over posterior uterine cavity wall | Tubercular Deposits Over Atrophic Endometrium |
 |
 |
| Adhesions in Endometrial tuberculosis | Adhesions Band – Endocervical Eanal |
 |
 |
| Starry Sky Appearance with Tubacle | A Bizarre Endometrial Architecture |
Hysteroscopy is a diagnostic tool diagnosing Endometrial Tuberculosis. It is performed to evaluate the intracavity, the severity of condition after treatment as a relook and as prognostic tools for future reproductive function.
References:
- News Flash. Current Tuberculosis Outbreak in Kansas City, K. Posted on: January 31, 2025
- Tuberculosis in Kansas: The Larger Picture | Johns Hopkins | Bloomberg School of Public Health
- Karen Dobos. As tuberculosis cases rise in the US and worldwide, health officials puzzle over the resurgence of a disease once in decline. Published: March 6, 2025
- Current Tuberculosis Outbreak in Kansas City, Kan. Metro Area. Kansas Health Alert Network (KS-HAN). News Flash • Current Tuberculosis Outbreak in Kansas City, K
- Global Tuberculosis Report. France: WHO; 2017.
- Sharma JB. Current diagnosis and management of female genital tuberculosis. J Obstet Gynaecol India 2015;65:362‑71.
- Kumar A, Kumar A. Endometrial tuberculosis. J Am Assoc Gynecol Laparosc 2004;11:2
- Kumar A, Kumar A. Unusual appearing tubercular deposits at hysteroscopy. J Minim Invasive Gynecol 2004;14:144
- Kumar A. Kumar A. Intraluminal tubal adhesions. Fertil Steril. 2008; 89(2): 434-5
- Kumar A, Kumar A. Hysteroscopic findings of starry sky appearance and impregnated cobwebs in endometrial tuberculosis. International Journal of Gynecology and Obstetrics 126 (2014) 280–281
- Kumar A. Kumar A. Relook hysteroscopy after anti tubercular therapy. Fertil Steril. 2008; 89(3): 701-2
- Kumar A. Kumar A. Surface architecture in endometrial tuberculosis. Article in press. JMIG
- Kumar A, Kumar A. Endometrial tuberculosis in a unicornuate uterus with a rudimentary horn. Article in press. JMIG
- Kumar A, Kumar A. Endometrial Tubercular Abscess. J Minim Invasive Gynecol. 2017 Feb 3. 24(7):1067-1068.
- Kumar A, Kumar A. Hysteroscopic Markers in Endometrial tuberculosis. Article in Keynote in Hysteroscopy. CBS 2019; 178-181
- Cicinelli et al. Tubercular Endometritis: A Rare Condition Reliably Detectable with Fluid Hysteroscopy JMIG. 2008; 15(6): 752)
About the Author:
Alka Kumar, MBBS, MS
 Dr. Kumar is the Chair of the AAGL Hysteroscopy Special Interest Group and Director of the Women’s Health Centre in Jaipur, Rajasthan, India.
Dr. Kumar is the Chair of the AAGL Hysteroscopy Special Interest Group and Director of the Women’s Health Centre in Jaipur, Rajasthan, India.
Difficult Lateral Metroplasty in Unicornuate Uterus: Surgical Challenges and Outcome
Hysteroscopic metroplasty is a minimally invasive procedure designed to correct uterine malformations that contribute to infertility, recurrent miscarriage, and other reproductive complications. The primary goal of the procedure is to convert a pear-shaped uterus into a triangular-shaped uterus, enhancing the uterine cavity for optimal pregnancy support. This is achieved by reshaping the uterine cavity through direct visualization and precision tissue resection via a hysteroscope.
Indications for Hysteroscopic Metroplasty
Hysteroscopic metroplasty is typically indicated in the following cases:
- T-shaped Uterus:
Often caused by exposure to diethylstilbestrol (DES), this condition results in lateral indentations of the uterine cavity, leading to infertility and recurrent miscarriages. Hysteroscopic metroplasty reshapes the uterine cavity to improve implantation and pregnancy retention.
2. Unicornuate Uterus:
A congenital anomaly where one of the paramesonephric ducts fails to develop, resulting in a single uterine horn. It can cause infertility, recurrent miscarriage, and ectopic pregnancy. Hysteroscopic metroplasty can be used to correct distortions in the uterine cavity, even in the absence of a rudimentary horn.
3. Recurrent Miscarriages:
Women with uterine malformations such as a septate uterus or T-shaped uterus often experience recurrent miscarriages due to anatomical distortions. Hysteroscopic metroplasty helps remove obstructive tissue and reshapes the cavity, improving pregnancy outcomes.
4. Infertility Due to Uterine Abnormalities:
Uterine malformations can obstruct sperm transport or disrupt embryo implantation. Hysteroscopic metroplasty corrects these abnormalities, increasing fertility and the likelihood of successful pregnancy.
Case Presentation: Hysteroscopic Metroplasty in Unicornuate Uterus
A 32-year-old woman with a history of infertility and recurrent pregnancy loss was diagnosed with a unicornuate uterus. Imaging confirmed the absence of a rudimentary horn (Fig. 1), but the uterine cavity exhibited significant distortion. Given these findings, hysteroscopic metroplasty was performed to correct the uterine shape and enhance reproductive potential.
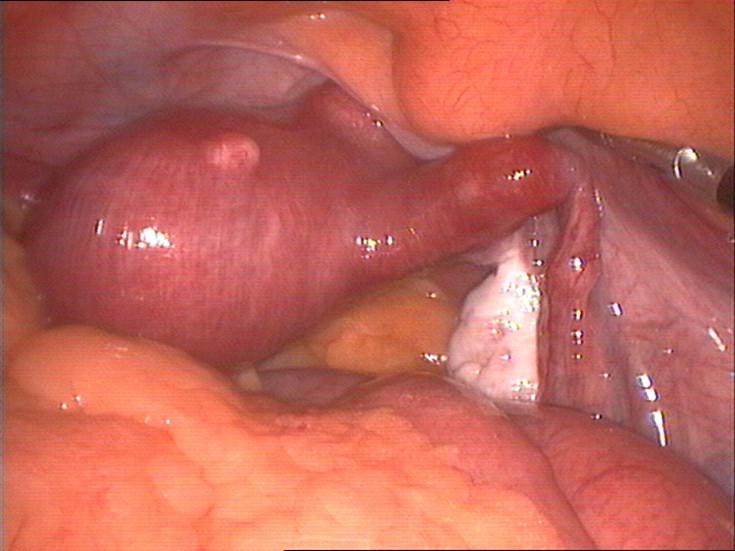 Figure 1. Unicornuate Uterus
Figure 1. Unicornuate Uterus
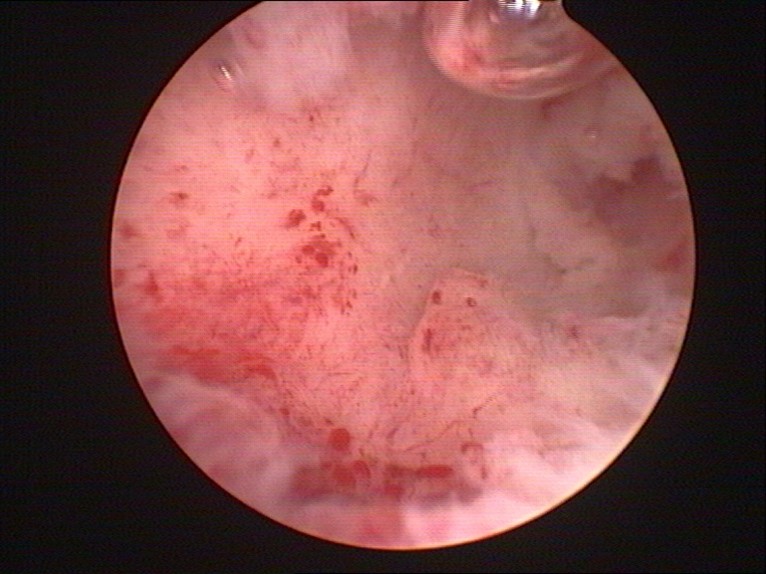 Figure 2. Hysteroscopic View of Unicornuate Uterus
Figure 2. Hysteroscopic View of Unicornuate Uterus
Surgical Challenges
- Uterine Distortion and Limited Space:
The unicornuate uterus showed anatomical distortion with lateral indentations, which restricted the available space for the hysteroscope. This posed challenges in visualizing and accessing all areas of the uterine cavity that required resection. - Resection of Uterine Tissue:
The tissue resection was performed using cold scissors and a Collin’s knife. The challenge was to carefully excise the lateral indentations without damaging surrounding uterine tissue, which is essential for preserving the patient’s fertility potential. - Residual Myometrial Thickness:
A key surgical challenge was managing residual myometrial thickness. The myometrium in a unicornuate uterus can be irregular in thickness. It was crucial to assess and avoid excessive resection to prevent uterine perforation while ensuring enough tissue removal to correct the distortion. - Risk of Uterine Perforation:
Given the distorted uterine anatomy, the risk of uterine perforation was heightened. Precise manipulation of instruments and controlled uterine distention were vital to avoid perforation and to perform a safe procedure. - Inadequate Visualization:
The distorted shape of the unicornuate uterus limited visualization during the procedure. To overcome this, high-quality hysteroscopic equipment and careful distention techniques were employed to optimize visualization and ensure proper resection.
Hysteroscopic metroplasty is an effective method for correcting uterine malformations such as unicornuate uterus. In this case, despite the absence of a rudimentary horn, the procedure successfully improved the uterine cavity structure, enhancing fertility potential. The surgical challenges, including uterine distortion, residual myometrial thickness, limited visualization, and the risk of uterine perforation, require meticulous planning and execution. With the use of precise instruments like cold scissors and Collin’s knife, hysteroscopic metroplasty offers a viable solution for correcting uterine anomalies and improving reproductive outcomes.
Postoperatively, the patient recovered without complications. Six months after the procedure, she conceived naturally and carried the pregnancy to term. Hysteroscopic metroplasty successfully corrected the uterine distortion, leading to a favorable reproductive outcome.
References
- Alonso Pacheco L, Laganà AS, Garzon S, et al. Hysteroscopic outpatient metroplasty for T-shaped uterus in women with reproductive failure: results from a large prospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2019;243:173–178. doi: 10.1016/j.ejogrb.2019.09.023. [DOI] [PubMed] [Google Scholar]
- Bermejo C, Martinez Ten P, Cantarero R, et al. Three-dimensional ultrasound in the diagnosis of Mullerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet Gynecol. 2010;35:593–601. doi: 10.1002/uog.7551. [DOI] [PubMed] [Google Scholar]
- Bettocchi S, Ceci O, Nappi L, et al. Office hysteroscopic metroplasty: three “diagnostic criteria” to differentiate between septate and bicornuate uteri. J Minim Invasive Gynecol. 2007;14:324–328. doi: 10.1016/j.jmig.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Boza A, Akin OD, Oguz SY, et al. Surgical correction of T-shaped uteri in women with reproductive failure: Long term anatomical and reproductive outcomes. J Gynecol Obstet Hum Reprod. 2019;48:39–44. doi: 10.1016/j.jogoh.2018.10.013. [DOI] [PubMed] [Google Scholar]
- Byrne J, Nussbaum-Blask A, Taylor WS, et al. Prevalence of Müllerian duct anomalies detected at ultrasound. Am J Med Genet. 2000;94:9–12. doi: 10.1002/1096-8628(20000904)94:1<9::aid-ajmg3>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Campo R, Santangelo F, Gordts S, et al. Outpatient hysteroscopy. Facts Views Vis Obgyn. 2018;10:115–122. [PMC free article] [PubMed] [Google Scholar]
- Casadio P, Gubbini G, Morra C, et al. Channel-like 360° isthmocele treatment with a 16 F mini-resectoscope: a step-by-step technique. J Minim Invasive Gynecol. 2019;26:1229–1230. doi: 10.1016/j.jmig.2019.04.024. [DOI] [PubMed] [Google Scholar]
- Di Spiezio Sardo A, Bettocchi S, Spinelli M, et al. Review of new office-based hysteroscopic procedures 2003-2009. J Minim Invasive Gynecol. 2010;17:436–448. doi: 10.1016/j.jmig.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Di Spiezio Sardo A, Campo R, Zizolfi B, et al. Long-term reproductive outcomes after hysteroscopic treatment of dysmorphic uteri in women with reproductive failure: an european multicenter study. J Minim Invasive Gynecol. 2020;27:755–762. doi: 10.1016/j.jmig.2019.05.011. [DOI] [PubMed] [Google Scholar]
- Di Spiezio Sardo A, Di Carlo C, Minozzi S, et al. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and meta-analysis. Hum Reprod Update. 2016;22:479–496. doi: 10.1093/humupd/dmw008. [DOI] [PubMed] [Google Scholar]
About the Authors:
Alka Kumar, MBBS, MS
Vidya V. Bhat, MBBS, MD, DNB


Dr. Kumar is Chair of the AAGL Hysteroscopy Special Interest Group and Director of the Women’s Health Centre in Jaipur, Rajasthan, India.
Dr. Bhat is Medical Director at the Radhakrishna Multispecialty Hospital and IVF Center in Bengaluru, Karnataka, India.

Hysteroscopy and Artificial Intelligence
The use of artificial intelligence for the diagnostic evaluation of medical images such as radiographic images with mimics analysis using genome data, and clinical information has been increasing in recent years. There have been increasing numbers of reports on the use of artificial intelligence in the field of gynecology. Despite the advancements in artificial intelligence across various medical fields, there has been relatively limited research specifically focusing on the application of AI for diagnosing endometrial lesions like endometrial hyperplasia, endometrial carcinoma. One of the popular methods for identifying endometrial lesions is hysteroscopy.
Hysteroscopy is, in general, considered the standard procedure for examining endometrial lesions by directly evaluating the uterine cavity. It is noteworthy that recent studies have suggested that hysteroscopy can be considered an effective technique for accurate endometrial-cancer diagnosis. Endometrial cancer is the most common gynecologic malignancy, and its incidence has increased significantly in recent years. Patients demonstrating early symptoms of the disease or suffering from low-risk endometrial cancer can be prescribed a favorable prognosis. Early diagnosis of endometrial cancer assumes paramount importance. Cervical cytology through pap smear is a common screening method employed in cervical cancer diagnosis.
Yu Takahashi et al (3) reported that machine learning techniques based on three popular deep neural network models were employed, and a continuity-analysis method was developed to enhance the accuracy of cancer diagnosis. They finally, we investigated if the accuracy could be improved by combining all the trained models.
Another study by F. Moro et al (2) proposes implements and evaluates an Artificial Intelligence (AI)-based prototype utilizing deep learning algorithms for endometrial lesions, which would increase the accuracy by acting as an assistant to the gynecologists. Specialized AI models demonstrate high precision and recall rates, significantly enhancing diagnostic capabilities. The proposed system here uses the advantage of completely developed object detection models, making use of multiple You Only Look Once (YOLO) versions, trained on a comprehensive dataset of hysteroscopy images annotated by surgeons. YOLO is a cutting- edge object detection algorithm.
The YOLO architecture is divided into three main components: the backbone, neck, and head. The backbone is a Convolutional Neural Network (CNN) that extracts and aggregates features from the input image. The neck further processes these features to optimize detection of objects by altering their sizes, from small to large. In the final stage, the head takes the processed features from the backbone and the neck in order to make the ultimate prediction, primarily by using convolutional layers. The study includes classification for four types of lesions: Endometrial Hyperplasia (EH), Endometrial Cancer (EC), Endometrial Polyp (EP), and Submucous Fibroid (SM).
Sergio Haimovich in a published article on LinkedIn in February 2025 (1) put forth key points related to AI and Hysteroscopy.
- Enhanced Diagnostics: Endometrial Cancer: AI systems now analyze subtle vascular patterns and integrate molecular markers to detect early cancer with higher sensitivity and specificity than traditional methods.
- Intrauterine Adhesions (IUAs): Al-enhanced scoring systems combine hysteroscopic visuals with patient factors (e.g., hormone levels, prior losses) to better predict fertility outcomes and guide treatment.
- Surgical Advancements: Preoperative Planning & Real-Time Guidance: Tools such as Fibroid Map AI and Hystero Vision create precise surgical blueprints and offer real-time overlays (highlighting safety margins and vascular maps), reducing operative time, blood loss, and complications during procedures like
- Fluid Management: Al predicts fluid overload well before clinical signs appear, helping to avoid complications such as
- Personalized Patient Care: Risk
- Postoperative Management.
- Educational and Training Innovations: Simulation & Certification.
- Ethical and Regulatory
Conclusion:
Artificial intelligence has the potential to convert subjective clinical practice into precise, data-driven medicine. Effective AI modules can enhance and standardize the diagnostic accuracy of hysteroscopy making safer and more accessible gynecologic care of women.
References
- Sergio Haimovich, et al. How artificial intelligence (AI) is transforming Published in LinkedIn on Feb 8, 2025; https://www.linkedin.com/pulse/how-artificial-intelligence-ai-transforming-sergio-haimovich-0j2of
- Moro et al. Application of artificial intelligence to ultrasound imaging for benign gynecological disorders: systematic review. Ultrasound Obstet Gynecol 2025 Published online in Wiley Online Library (wileyonlinelibrary.com). DOI: 10.1002/uog.29171.
- Yu Takahashi et al. Automated system for diagnosing endometrial cancer by adopting deep learning technology in hysteroscopy. PLOS ONE | https://doi.org/10.1371/journal.pone.0248526 March 31, 2021
About the Authors:
Erkut Attar, MD
Alka Kumar, MBBS, MS


Dr. Attar is Chair of the Department of Obstetrics and Gynecology and Head of the IVF and Infertility Unit at Yeditepe University Medical School in Istanbul.
Dr. Kumar is Chair of the AAGL Hysteroscopy Special Interest Group and Director of the Women’s Health Centre in Jaipur, Rajasthan, India.
The post Spotlight On: Hysteroscopy appeared first on NewsScope.